What is in vitro fertilization (IVF)?

Benefits of IVF
Success in various types of infertility: IVF is recognized as an effective method for treating infertility cases that have not responded to other treatments.
Ability to use donor eggs, sperm, or embryos: This method allows for the use of donated eggs, sperm, or embryos to achieve pregnancy.
An option for couples with complex infertility issues: IVF can be successful in cases of unexplained infertility or when multiple infertility factors are present.
Genetic disease diagnosis and prevention: Through techniques like preimplantation genetic diagnosis (PGD), embryos can be screened for genetic abnormalities, helping to prevent certain inherited diseases.
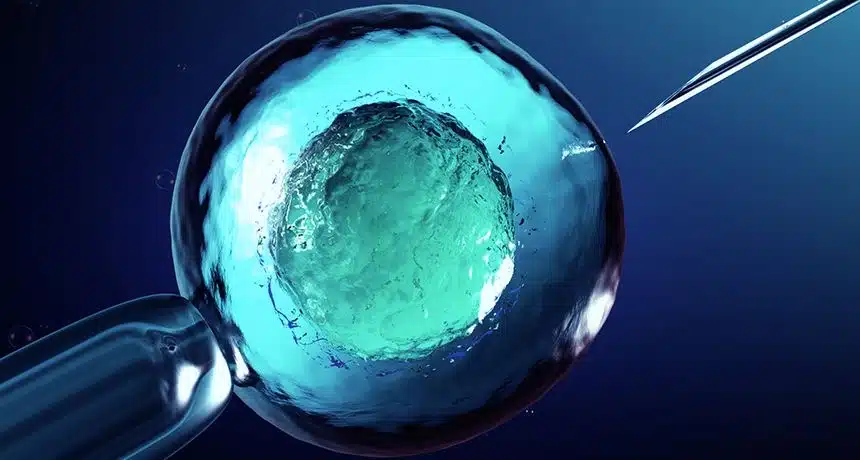
IVF (In Vitro Fertilization) is an assisted reproductive method in which egg and sperm are fertilized in a laboratory environment outside the woman's body. This method is especially used for couples who are facing infertility problems and are not able to conceive naturally. IVF helps to create the conditions in which the egg and sperm combine to form an embryo. After that, the embryo is transferred to the woman's uterus to start a natural pregnancy.
IVF procedure
Diagnosis and evaluation of infertility: Before starting IVF, necessary tests and evaluations are conducted to diagnose the cause of infertility.
Ovarian stimulation: Hormonal medications are prescribed to the woman to stimulate the ovaries and produce multiple mature eggs. This stage usually lasts between 10 to 14 days and is intended to increase the chances of successful fertilization.
Egg retrieval: Once the eggs have matured, they are collected from the ovaries using a special needle under ultrasound guidance. This process is known as ovarian puncture and is performed under local or general anesthesia.
Laboratory fertilization: The collected eggs are combined with sperm provided by the man in a laboratory environment. Fertilization naturally occurs in culture dishes, and the fertilized eggs begin to divide and form embryos.
Embryo culture and growth: The embryos resulting from fertilization are grown in special culture environments for a few days. During this time, embryologists monitor the embryos for quality and development, selecting the best ones for transfer to the uterus.
Embryo transfer to the uterus: After a few days, healthy and high-quality embryos are transferred to the woman’s uterus. This step is performed using a thin catheter and does not require surgery or anesthesia. If the embryo successfully attaches to the uterine wall, pregnancy begins.
IVF is specifically used in the following situations:
Blocked or damaged fallopian tubes: When a woman's fallopian tubes are blocked or damaged, IVF can be a suitable option for achieving pregnancy.
Unexplained infertility: In cases where the cause of infertility is unknown, IVF can increase the chances of conception.
Ovulation problems: For women who do not ovulate regularly or have a low egg count, IVF can help facilitate pregnancy.
Male infertility: In situations where the sperm count is low, sperm motility is poor, or the sperm are unable to reach the egg, IVF can assist in fertilization.
Use of donor eggs or sperm: IVF is also an option when donor eggs or sperm are used for conception.
Use of frozen embryos: In cases where frozen embryos from previous fertility treatments are available, they can be used for future pregnancy attempts.
IVF treatment process
Differences Between IVF and ICSI
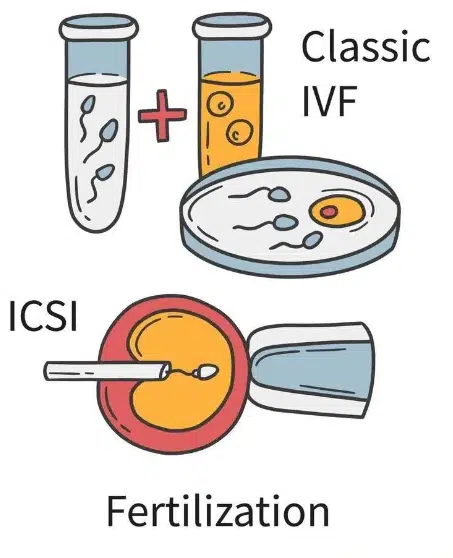
In vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI) are both advanced assisted reproductive technologies used to increase the chances of pregnancy for couples facing infertility issues. However, these two methods have key differences in how they are performed and when they are used.
In IVF, eggs and sperm are placed in a controlled laboratory environment to allow for natural fertilization. The sperm must actively penetrate the egg to fertilize it, meaning the fertilization occurs naturally without direct intervention.
IVF is suitable for women with infertility issues such as blocked or damaged fallopian tubes, ovulation disorders, or unexplained infertility. It is also appropriate when sperm quality is adequate, eliminating the need for direct injection of sperm into the egg.
In ICSI, a single sperm is injected directly into the cytoplasm of the egg. This method is used to ensure fertilization in cases where sperm cannot penetrate the egg naturally, or when there are low numbers or poor quality of sperm. ICSI is particularly beneficial for men with severe infertility issues, such as very low sperm count, poor sperm motility, or abnormal sperm shape. It is also utilized when there have been repeated failures in fertilization using IVF or when low-quality frozen sperm is used.
The success rate of IVF depends on the quality of the eggs and sperm as well as other factors, while ICSI tends to have higher success rates in cases of male infertility because the sperm is directly injected into the egg.
In terms of cost and complexity, ICSI is more expensive and complex due to the use of advanced technologies, whereas IVF is a simpler process.
Although both methods are safe, IVF may have complications such as ovarian stimulation and multiple pregnancies, while ICSI carries a slight risk of genetic issues.
